Back Pain
Back pain can range in intensity from a dull, constant ache to a sudden, sharp or shooting pain. It can begin suddenly as a result of an accident or by lifting something heavy, or it can develop over time as we age. Getting too little exercise followed by a strenuous workout also can cause back pain.
There are two types of back pain:
Acute, or short-term back pain lasts a few days to a few weeks. Most low back pain is acute. It tends to resolve on its own within a few days with self-care and there is no residual loss of function. In some cases a few months are required for the symptoms to disappear.
Chronic back pain is defined as pain that continues for 12 weeks or longer, even after an initial injury or underlying cause of acute low back pain has been treated. About 20 percent of people affected by acute low back pain develop chronic low back pain with persistent symptoms at one year. Even if pain persists, it does not always mean there is a medically serious underlying cause or one that can be easily identified and treated. In some cases, treatment successfully relieves chronic low back pain, but in other cases pain continues despite medical and surgical treatment.
At Aptiva Health, we offer same-day and walk-in appointments for spine injuries and conditions to evaluate, diagnose, and make the appropriate referral for additional treatment based upon your specific spine injury or condition. We treat spine injuries and conditions in our Spine, Pain Management, General Medicine, Orthopedics, and Physical Therapy departments.
Causes
Most acute low back pain is mechanical in nature, meaning that there is a disruption in the way the components of the back (the spine, muscle, intervertebral discs, and nerves) fit together and move. Some examples of mechanical causes of low back pain include:
Congenital
Skeletal irregularities such as scoliosis (a curvature of the spine), lordosis (an abnormally exaggerated arch in the lower back), kyphosis (excessive outward arch of the spine), and other congenital anomalies of the spine.
Spina bifida which involves the incomplete development of the spinal cord and/or its protective covering and can cause problems involving malformation of vertebrae and abnormal sensations and even paralysis.
Injuries
Sprains (overstretched or torn ligaments), strains (tears in tendons or muscle), and spasms (sudden contraction of a muscle or group of muscles)
Traumatic Injury such as from playing sports, car accidents, or a fall that can injure tendons, ligaments, or muscle causing the pain, as well as compress the spine and cause discs to rupture or herniate.
SI Joint Dysfunction can cause pain anywhere in the lower back or spine, buttocks, pelvis, groin, or sometimes in the legs. SI joint pain symptoms can be caused by an acute trauma (like a motor vehicle collision or pregnancy) or from joint degeneration.
Nerve and spinal cord problems
Spinal nerve compression, inflammation and/or injury
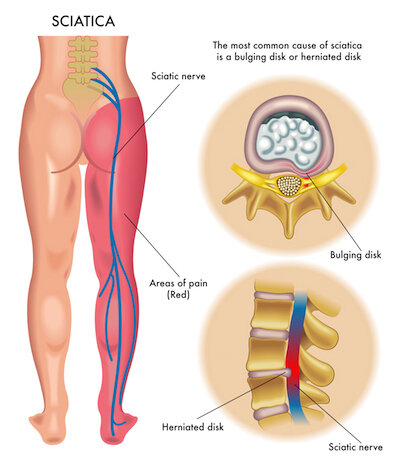
Sciatica (also called radiculopathy), caused by something pressing on the sciatic nerve that travels through the buttocks and extends down the back of the leg. People with sciatica may feel shock-like or burning low back pain combined with pain through the buttocks and down one leg.
Spinal stenosis, the narrowing of the spinal column that puts pressure on the spinal cord and nerves.
Spondylolisthesis, which happens when a vertebra of the lower spine slips out of place, pinching the nerves exiting the spinal column.
Herniated or ruptured discs can occur when the intervertebral discs become compressed and bulge outward.
Infections involving the vertebrae, a condition called osteomyelitis; the intervertebral discs, called discitis; or the sacroiliac joints connecting the lower spine to the pelvis, called sacroiliitis
Cauda equina syndrome occurs when a ruptured disc pushes into the spinal canal and presses on the bundle of lumbar and sacral nerve roots. Permanent neurological damage may result if this syndrome is left untreated.
Myelopathy is an injury to the spinal cord caused by severe compression that may be a result of spinal stenosis, disc degeneration, disc herniation, autoimmune disorders or other trauma. When any part of the spinal cord is compressed, it causes nerve dysfunction along the spinal cord resulting in pain, loss of balance and coordination and numbness in the area around the compression point.
Osteoporosis (a progressive decrease in bone density and strength that can lead to painful fractures of the vertebrae)
Degenerative problems
Intervertebral disc degeneration which occurs when the usually rubbery discs wear down as a normal process of aging and lose their cushioning ability.
Spondylosis the general degeneration of the spine associated with normal wear and tear that occurs in the joints, discs, and bones of the spine as people get older.
Arthritis or other inflammatory disease in the spine, including osteoarthritis and rheumatoid arthritis as well as spondylitis, an inflammation of the vertebrae.
Diagnosis
A complete medical history and physical exam can usually identify any serious conditions that may be causing the pain. Neurologic tests can help determine the cause of pain and appropriate treatment. Imaging tests are not needed in most cases but may be ordered to rule out specific causes of pain, including tumors and spinal stenosis. Occasionally the cause of chronic lower back pain is difficult to determine even after a thorough examination.
Tests include:
Blood tests are not routinely used to diagnose the cause of back pain but might be ordered to look for signs of inflammation, infection, cancer, and/or arthritis.
Bone scans can detect and monitor an infection, fracture, or bone disorder. A small amount of radioactive material is injected into the bloodstream and collects in the bones, particularly in areas with some abnormality. Scanner-generated images can identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.
Discography involves injecting a contrast dye into a spinal disc thought to be causing low back pain. The fluid’s pressure in the disc will reproduce the person’s symptoms if the disc is the cause. The dye helps to show the damaged areas on CT scans taken following the injection.
Electrodiagnostics can identify problems related to the nerves in the back and legs. The procedures include:
Electromyography (EMG) assesses the electrical activity in a muscle and can detect if muscle weakness results from a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body.
Evoked potential studies involve two sets of electrodes—one set to stimulate a sensory nerve, and the other placed on the scalp to record the speed of nerve signal transmissions to the brain.
Nerve conduction studies (NCS) also use two sets of electrodes to stimulate the nerve that runs to a particular muscle and record the nerve’s electrical signals to detect any nerve damage.
Diagnostic imaging tests allow specialists to see into the body without having to perform exploratory surgery. Imaging includes:
Computerized tomography (CT) can show soft tissue structures that cannot be seen on conventional x-rays, such as disc rupture, spinal stenosis, or tumors.
Magnetic resonance imaging (MRI) creates a computer-generated image of bony structures and soft tissues such as muscles, ligaments, tendons, and blood vessels. An MRI may be ordered if a problem such as infection, tumor, inflammation, disc herniation or rupture, or pressure on a nerve is suspected
X-ray imaging can show broken bones or an injured or misaligned vertebra.
Myelograms enhance the diagnostic imaging of x-rays and CT scans. In this procedure, a contrast dye is injected into the spinal canal, allowing spinal cord and nerve compression caused by herniated discs or fractures to be seen on an x-ray or CT scans.
Treatment
Step 1 Early Treatment Options:
Medications may include:
Analgesics and NSAIDS
Opioid medications prescribed by a physician (opioids should be used only for a short period of time and under a physician’s supervision, as opioids can be addictive, aggravate depression, and have other side effects)
Anticonvulsants—prescribed drugs primarily used to treat seizures—may be useful in treating people with sciatica
Antidepressants such as tricyclics and serotonin, and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain (prescribed by a physician)
Self-management:
Hot or cold packs
Resuming normal activities as soon as possible may ease pain; bed rest is not recommended
Exercises that strengthen core or abdominal muscles may help to speed recovery from chronic low back pain. Always check first with a physician before starting an exercise program and to get a list of helpful exercises.
Step 2 Conservative Treatment Options:
Transcutaneous electrical nerve stimulation (TENS) involves wearing a battery-powered device which places electrodes on the skin over the painful area that generate electrical impulses designed to block or modify the perception of pain
Physical therapy programs to strengthen core muscle groups that support the low back, improve mobility and flexibility, and promote proper positioning and posture are often used in combination with other interventions
Traction involves the use of weights and pulleys to apply constant or intermittent force to gradually “pull” the skeletal structure into better alignment. Some people experience pain relief while in traction but the back pain tends to return once the traction is released.
Spinal manipulation and spinal mobilization are approaches in which doctors of chiropractic care use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques may provide small to moderate short-term benefits in people with chronic low back pain but neither technique is appropriate when a person has an underlying medical cause for the back pain such as osteoporosis, spinal cord compression, or arthritis.
Dry needling is moderately effective for chronic low back pain. It involves inserting thin needles into precise points throughout the body and stimulating them (by twisting or passing a low-voltage electrical current through them), which may cause the body to release naturally occurring painkilling chemicals such as endorphins, serotonin, and acetylcholine.
Step 3 Interventional Injection Therapy:
Interventional pain management injections to include:
Trigger point injections can relax knotted muscles (trigger points) that may contribute to back pain. An injection or series of injections of a local anesthetic and often a corticosteroid drug into the trigger point(s) can lessen or relieve pain.
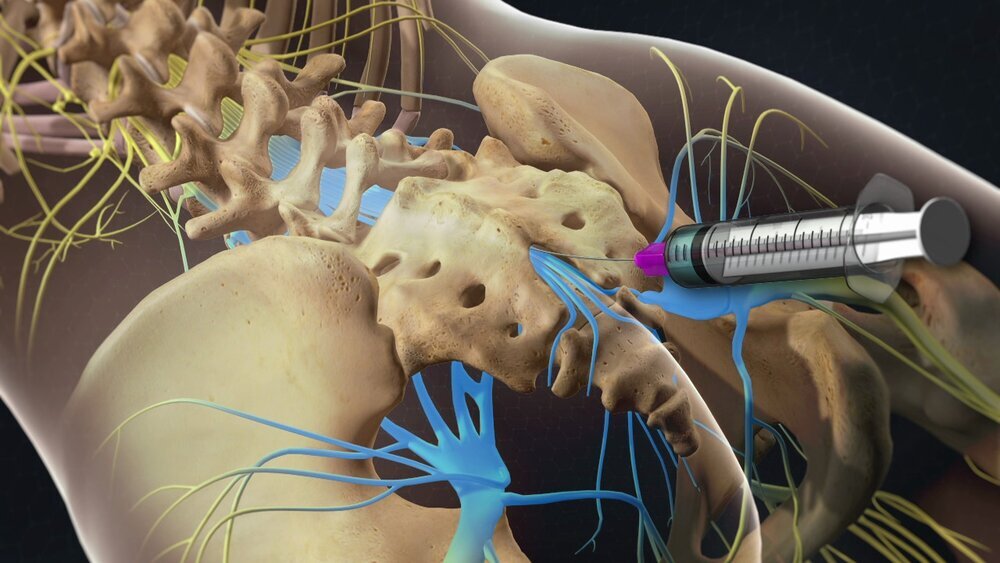
Epidural steroid injections into the lumbar area of the back are given to treat low back pain and sciatica associated with inflammation. Pain relief associated with the injections tends to be temporary and the injections are not advised for long-term use.
Facet Joint Injections. The facet joints are small joints in the back of the spine that form connections between each vertebra. If these joints are blocked or numbed, they will not be able to transfer the painful sensation to the brain. Therefore, this procedure is completed to see if your back (or neck) pain is caused by the facet joints.
SI Joint Injections. Sacroiliac (SI) joint pain is easily confused with back pain from the spine. Sometimes injecting the SI joint with lidocaine may help your doctor determine whether the SI joint is the source of your pain. If the joint is injected and your pain does not go away, it may be coming from a different source. During the procedure, a mixture of local anesthetic and steroid is injected into the SI joint. The local anesthetic will numb the area, and steroid may help lower the swelling. The steroid should reduce the pain and improve the motion in your hip or buttock.
Medial branch block injection is used to determine if the facet joint is causing the patient's back pain. Facet joints are pairs of small joints between the vertebrae in the back of the spine.
Radiofrequency ablation involves inserting a fine needle into the area causing the pain through which an electrode is passed and heated to destroy nerve fibers that carry pain signals to the brain. Also called a rhizotomy, the procedure can relieve pain for several months.
Step 4 Surgical Intervention
When other therapies fail, surgery may be considered to relieve pain caused by worsening nerve damage, serious musculoskeletal injuries, or nerve compression. Specific surgeries are selected for specific conditions/indications. Surgical options include:
Vertebroplasty and kyphoplasty for fractured vertebra are minimally invasive treatments to repair compression fractures of the vertebrae caused by osteoporosis. Vertebroplasty uses three-dimensional imaging to assist in guiding a fine needle through the skin into the vertebral body, the largest part of the vertebrae. A glue-like bone cement is then injected into the vertebral body space, which quickly hardens to stabilize and strengthen the bone and provide pain relief. In kyphoplasty, prior to injecting the bone cement, a special balloon is inserted and gently inflated to restore height to the vertebral structure and reduce spinal deformity.
Spinal laminectomy (also known as spinal decompression) is done when a narrowing of the spinal canal causes pain, numbness, or weakness. During the procedure, the lamina or bony walls of the vertebrae are removed, along with any bone spurs, to relieve pressure on the nerves.
Discectomy and microdiscectomy involve removing a herniated disc through an incision in the back (microdiscectomy uses a much smaller incision in the back and allows for a more rapid recovery). Laminectomy and discectomy are frequently performed together and the combination is one of the more common ways to remove pressure on a nerve root from a herniated disc or bone spur.
Foraminotomy is an operation that “cleans out” or enlarges the bony hole (foramen) where a nerve root exits the spinal canal. Bulging discs or joints thickened with age can narrow the space where the spinal nerve exits and press on the nerve. Small pieces of bone over the nerve are removed through a small slit, allowing the surgeon to cut away the blockage and relieve pressure on the nerve.
Nucleoplasty, also called plasma disc decompression (PDD), is a type of laser surgery that uses radiofrequency energy to treat people with low back pain associated with mildly herniated discs. Under x-ray guidance, a needle is inserted into the disc. A plasma laser device is then inserted into the needle and the tip is heated to 40-70 degrees Celsius, creating a field that vaporizes the tissue in the disc, reducing its size and relieving pressure on the nerves.
Spinal fusion is used to strengthen the spine and prevent painful movements in people with degenerative disc disease or spondylolisthesis (following laminectomy). The spinal disc between two or more vertebrae is removed and the adjacent vertebrae are “fused” by bone grafts and/or metal devices secured by screws. Spinal fusion may result in some loss of flexibility in the spine and requires a long recovery period to allow the bone grafts to grow and fuse the vertebrae together. Spinal fusion has been associated with an acceleration of disc degeneration at adjacent levels of the spine.
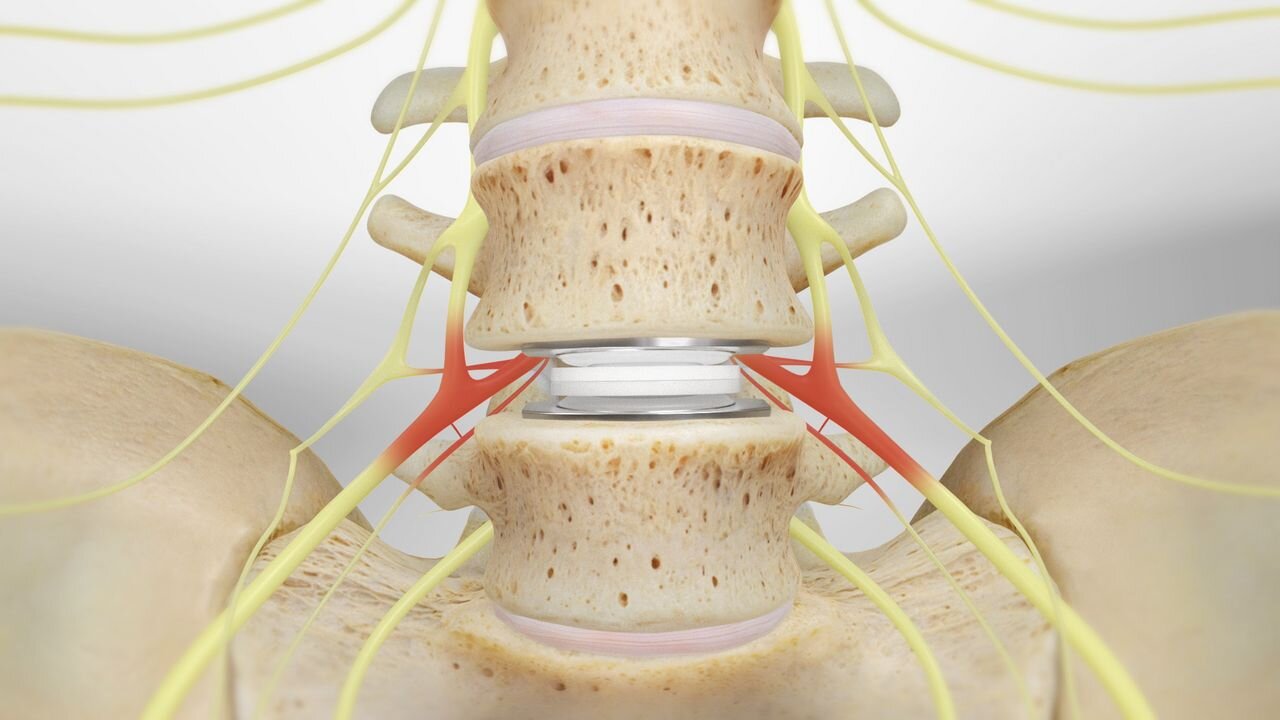
Artificial disc replacement is an alternative to spinal fusion for treating severely damaged discs. The procedure involves removing the disc and replacing it with a synthetic disc that helps restore height and movement between the vertebrae.
SI-Joint fusion. The goal of this procedure is to completely eliminate movement at the sacroiliac joint by grafting together the ilium and sacrum. Sacroiliac fusion involves the use of implanted screws or rods, as well as a possible bone graft across the joint. Minimally-invasive procedures have been developed in recent years that improve outcomes in pain and disability, and reduce recovery time.
Interspinous spacers are small devices that are inserted into the spine to keep the spinal canal open and avoid pinching the nerves. It is used to treat people with spinal stenosis.
Implanted nerve stimulators
Spinal cord stimulation uses low-voltage electrical impulses from a small implanted device that is connected to a wire that runs along the spinal cord. The impulses are designed to block pain signals that are normally sent to the brain.
Dorsal root ganglion stimulation also involves electrical signals sent along a wire connected to a small device that is implanted into the lower back. It specifically targets the nerve fibers that transmit pain signals. The impulses are designed to replace pain signals with a less painful numbing or tingling sensation.
Peripheral nerve stimulation also uses a small implanted device and an electrode to generate and send electrical pulses that create a tingling sensation to provide pain relief.